Indian Health Services (IHS): A Quick Primer
Prior to 1849 the responsibility for providing healthcare to the Native American population fell to the War Department. After 1849 that duty went to the newly created Bureau of Indian Affairs, the federal department in charge of managing the over 55MM acres of federal lands held in trust for Native Americans and Alaskan tribes.
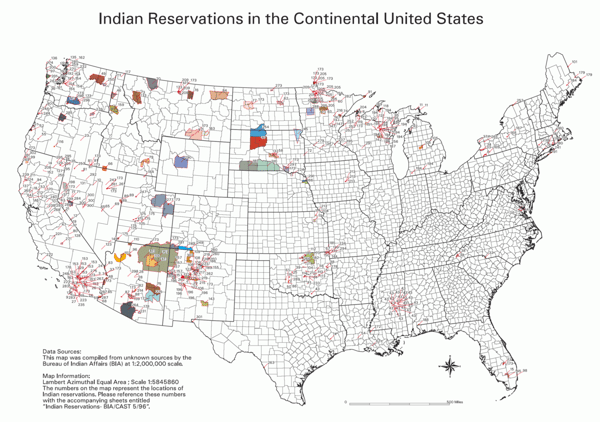
Fast forward to 1921 and the passage of the Snyder Act. This piece of legislation provided for “the relief of distress and conservation of health among American Indians.” As more changes in management and direction occurred, Congress created the Department of Health, Education and Welfare in 1953, and IHS started in earnest in 1955. The IHS is now under the Department of Health and Human Services and has an annual budget of $5.9B. IHS provides care for approximately 60% of the nation’s estimated 4 million American Indians and Alaska Natives. The majority live on or near reservations and rural communities. Most of these communities are in the western U.S. and Alaska.
IHS manages:
-
28 hospitals;
-
62 health centers;
-
25 health stations;
-
33 urban Indian health projects.
Additionally, individual American Indian Tribes and Alaska Native corporations manage:
-
18 hospitals;
-
282 health centers;
-
80 health stations;
-
150 Alaska village clinics.
Not the Picture of Health
Compared with other Americans, the American Indian and Alaska Native Tribes have poorer overall health. Life expectancy is four years shorter than the general population and the death rate is significantly higher. This includes deaths related to chronic liver disease and cirrhosis, and diabetes. Diabetes is incredibly prevalent in Native American populations. They have the highest rates of Type 2 diabetes in the United States. In fact, members of the Pima tribe in Arizona, have the highest rate of Type 2 diabetes in the world: 34.2% for men and 40.8% for women. Compare that to 9.3% of the general population of the United States. With the improvement in technologies and treatment paradigms, the potential to significantly improve the outcomes of these patients is real.
Telemedicine can help
Thomas Miller, PhD, ABPP, Professor Emeritus & Senior Research Scientist, InCHIP, University of Connecticut said, “Diabetes is particularly well-suited to the advantages of technology.” This is because it is a chronic condition that benefits from the constant monitoring and sharing of data that is easy to gather with current technology and medical devices that can integrate with telemedicine. There is also a strong connection between diabetes and depression, and telemedicine has been successfully used in many areas of behavioral health. This is especially helpful when implementing a multi-specialty approach. The whole patient must be treated, not just their blood sugars.
Keeping blood sugars lower and in tighter control has shown a significant decrease in the risk of heart attack and stroke. A Journal of Diabetes Technology & Therapeutics study from August of 2017 demonstrated the success of telemedicine in the treatment of Type 2 diabetes in rural patients with low income and poorly controlled diabetes. The rates of hemoglobin A1C (HbA1c), a marker used to measure long-term blood sugar levels, were significantly lower and the rate of decline of HbA1c was faster. A Centers for Disease Control (CDC) study also looked at telemedicine as part of the treatment program for rural veterans diagnosed with Type 1 diabetes and found that using telemedicine saved the patient time, money and improved appointment adherence and satisfaction rates.
The whole patient must be treated, not just their blood sugars.
IHS leaders know that telemedicine has value with their patients. Mary L. Smith, the IHS principal deputy director said, “It is challenging to provide specialty healthcare in rural areas, and this is especially true in Indian Country. IHS has long been a leader in information technology and electronic health records, and IHS experience shows that telemedicine is an effective way to increase access to quality health care services in remote, hard to reach areas.” Dr. Jonathan Gilbert, clinical director for the Billings-area office of IHS believes telemedicine is going to have a prominent role in the years to come. He sees it as a way to bring the much needed expertise of medical specialists to IHS rural patients. Chris Fore, PhD the director of the IHS TeleBehavioral Health Center of Excellence noted that when his peers gathered at conferences and discussed telemedicine, the discussion usually revolved around telemedicine’s general effectiveness. Now research is showing, “in some cases, it may be better than in person.”
An example of IHS embracing telemedicine can be seen within the Phoenix Area IHS (Arizona, California, Nevada, Utah). The Phoenix Area IHS has a group of ophthalmologists who assist other IHS facilities around the country that do not have opthamologists of their own. They participate by interpreting eye exam results taken from around the country as part of an established diabetic screening process. By using this ophthalmology group in Phoenix the participating IHS facilities can use a tech to administer the test. This means a significant savings while ensuring quality healthcare.
Opportunity Awaits!
While parts of the Phoenix Area IHS and Great Plains Area IHS are finding success with telemedicine, other IHS areas are still struggling with providing just basic internet access. This may be why the results of a survey of 40 IHS sites completed in 2014 by The National Emergency Department Inventory showed only 11% using telemedicine.
The Nez Perce tribe in north-central Idaho is a small community with almost no broadband services. Tribal members often end up driving up to six miles or more to find an internet connection. This does not bode well for the opportunity to adopt telemedicine into their community. According to the most recent report by the Federal Communications Commission (FCC) approximately 35 percent of Americans who live on tribal lands do not have any broadband access. The FCC estimates 83 percent of Nez Perce tribal members do not have access to broadband internet. This makes them one of the poorest connected populations in the country.
As the federal government and local tribal governments and communities continue making inroads into improving the connectivity of the Native American population, telemedicine is perfectly positioned to become a significant part of the overall treatment strategy for these patients by giving them the tools they can use to keep their blood sugar levels in check, improve their quality of life, and ultimately live longer, healthier lives.





