In our devotion to our customers, its important for the eVisit team to stay abreast of our fast-paced industry. It’s crucial to know the major happenings to help us serve as subject matter experts in virtual care and telehealth. Our industry is moving at warp speed and we work hard to stay in-the-know, and want to keep our blog readers up-to-date too. Since our last Insights Report, these are some top headlines in this quick-read post.
Use of Telehealth Stabilizing
The use of telehealth has “stabilized” at 38-times the rate it was being utilized pre-pandemic, according to a McKinsey report and as reported by HealthLeaders. Overall telehealth use for office visits and outpatient care was 78 times higher in April 2020 than in February 2020. Last year’s surge in telehealth’s use was driven by a number of important factors: the pandemic, which shut down in-person care, heightened willingness by patients and providers to use telehealth and the availability of federal reimbursements for virtual visits. Since the high-water mark, “utilization levels have largely stabilized, ranging from 13% to 17% across all specialties.” Check out the full McKinsey Report here.
A few more stats to share on this topic. According to the American Telemedicine Association (ATA) Edge Conference earlier this year, providers are planning and financially budgeting for a larger percentage of virtual care, between 10-30%. Americans are increasingly at ease with virtual visits, with one recent HIMSS Survey showing that 77% of consumers willing to use some form of telehealth post-COVID.
The Top 25 Hospitals Using Telehealth + What They Charged
The healthcare research firm, Hospital Pricing Specialists, analyzed more than 250 million Medicare hospital outpatient claims from April 1- Dec. 20, 2020, to determine the top 25 hospitals in the U.S. that offered telehealth services during the pandemic. Hospital outpatient visits accounted for more than 47% of the total claims. On the high end, Dana-Faber Institute in Boston averaged $487.30 per telehealth visit and on the low side, Carilion Roanoke Memorial Hospital in VA averaged $20 per visit. See the full list of the Top 25 at Becker’s Hospital Review.
Video Visits vs. Virtual Care — The Differences Are More Than Just in the Names
Most healthcare leaders, providers, and practice groups smartly jumped into offering telehealth with video visits when the coronavirus pandemic hit the U.S. last March.
This was a solid move. These healthcare professionals knew serving the needs of patients was paramount; with the regulatory barriers lifted, two-way video conferencing quickly met the immediate requirements to safely engage and deliver patient care.
This online Physician’s Practice story references a hospital system that was conducting 7,000+ video visits per month during the pandemic using a two-way video solution. They quickly learned what they needed: an efficient end-to-end solution that virtualizes every aspect of the clinical workflow from scheduling and intake, the remote visit itself, to ePrescribe, discharge, and payment.
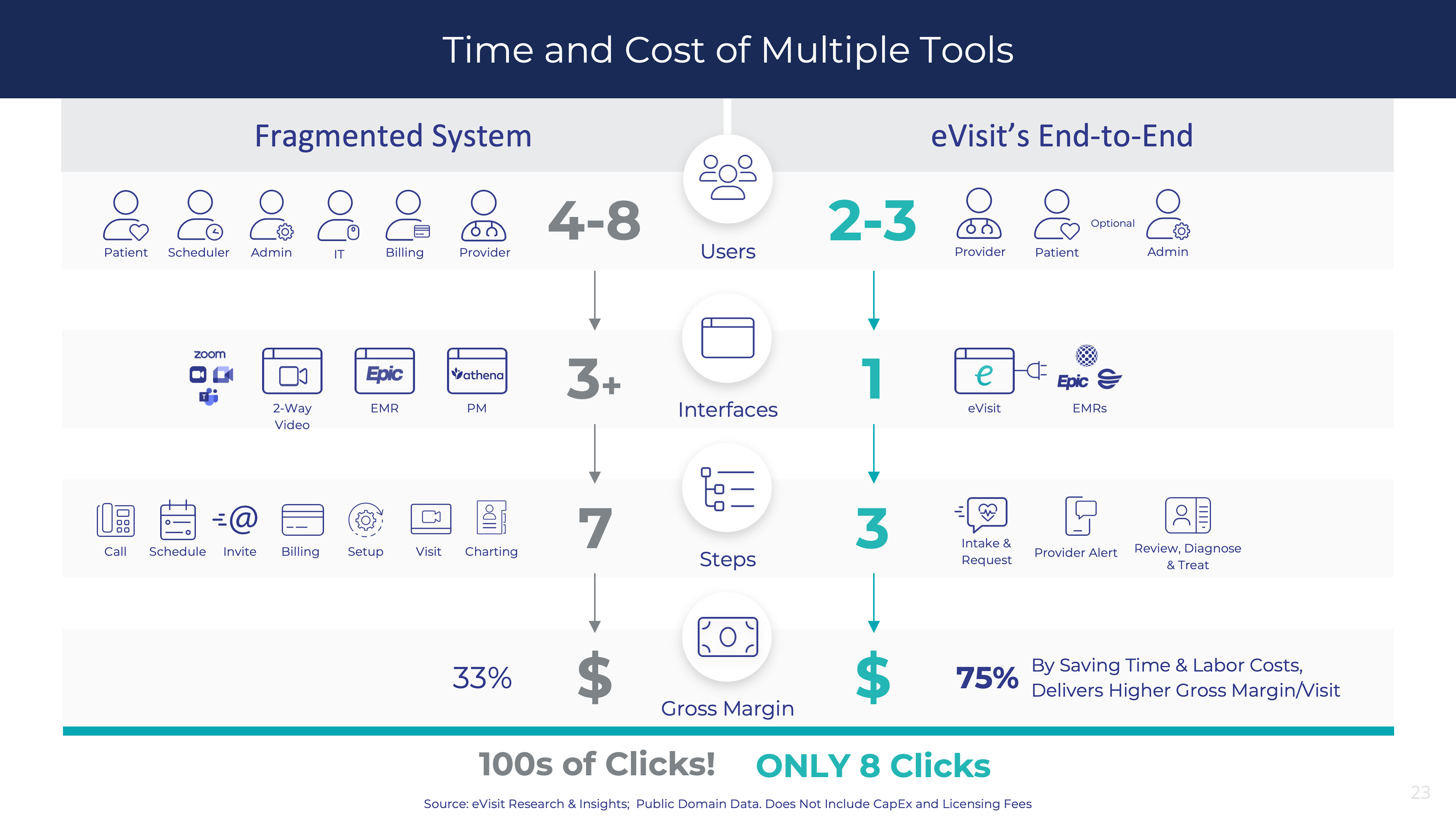
It also shares the above infographic which shows the significant disparity, especially the many friction points providers and staff encounter as they marry the myriad “non-virtualized” physical steps with the many team members it takes to conduct a single video visit for just one patient. Analysis show that using an end-to-end solution saves time and labor costs and delivers a higher gross margin/visit as high as 75%. Read the full story at PhysiciansPractice.com.
One Physician’s Perspective: Why Patients Prefer Telehealth Visits
An occupational medicine physician worked for an organization that assumed face-to-face interaction was the preferred healthcare experience and telehealth dehumanized the medical encounter. Then COVID hit and Dr. Archie Adams performed 90% of his visits via telehealth during the first 4 months of the pandemic. Dr. Adams surveyed his patients with one question: Considering the current pandemic, would you prefer a virtual visit or an in-person visit?
Here is what Dr. Adams learned as reported in his bylined piece in Healthcare IT News:
- 60% of in-person patients preferred a virtual encounter
- 86% wanted their future visits to remain virtual
- “I like the first visit to be in-person but follow ups can be virtual.”
- “Virtual is good, but when I had that spasm last time, I preferred in-person so you could feel it.”
- “I’m an essential worker, so virtual visits are convenient for me.”
- “I kinda like this, this is the collateral beauty of the pandemic.”
Dr. Adams also shares some tips. Having a robust and easy-to-use telehealth software that is HIPAA compliant is critical. Consider grouping telehealth visits and in-person visits on separate days for better workflow – what the industry is calling hybrid care.
We couldn’t agree more!
Click the button below to Schedule a consult with a Virtual Care Consultant at eVisit to learn more about our end-to-end eVisit Enterprise Virtual Care Platform and where you are on the Virtual Care Maturity Model.
Click the button below to learn more from our team of Virtual Care Consultants. Learn more at eVisit.com.
Stay in-the-know and subscribe to the Virtual Care Blog at the button below.




