What is medical office workflow and what does a good one look like?
No practice is 100% efficient, so every medical office has room for improvement. But where to begin? The easiest way to improve your medical office workflow is to figure out what needs work.
In any office, there are day-to-day frustrations everyone faces, and then there are specific bad habits that your staff can remedy with a little time and focus.
Pamela Moore at Physician's Practice explains workflows and how to make them more efficient. "The goal is to avoid waiting for someone else to do their job so you can do yours," Moore writes. She uses McDonald's as an example of optimal efficiency. "When an order comes in, the fry guy drops a basket in the fryer, the burger girl flips a patty, and the clerk rings up the sale and fills a soda, while the customer fumbles for change. They don't need to coordinate. No one forgets the pickles. Everything is ready when it needs to be."
Roles are distinguished, resources are always ready to go, and no two people do the exact same job. Your medical practice can be just as quick and precise, as long as you root out your problems first.
Here are some common flaws you may see in your practice and how to improve workflow in your medical office.
-
Do staff and patients seem to repeat themselves?
Do members of your office staff start a task, only to be told partway through that someone else has already completed it? Do your patients complain of giving the same information to three different staff members in one visit? If these are common problems in your practice, you may need to adjust your workflow.
Think through the path a typical patient would take at your office. Will your patient have to visit the front desk multiple times, or loop back to certain locations throughout one visit? Do you have patients give information in an exam room that could be provided at the start of a visit, freeing up valuable treatment space? And, when your patient leaves, do they have clear direction from the doctor and office staff for future visits, or do they call the office when they're home to ask questions?
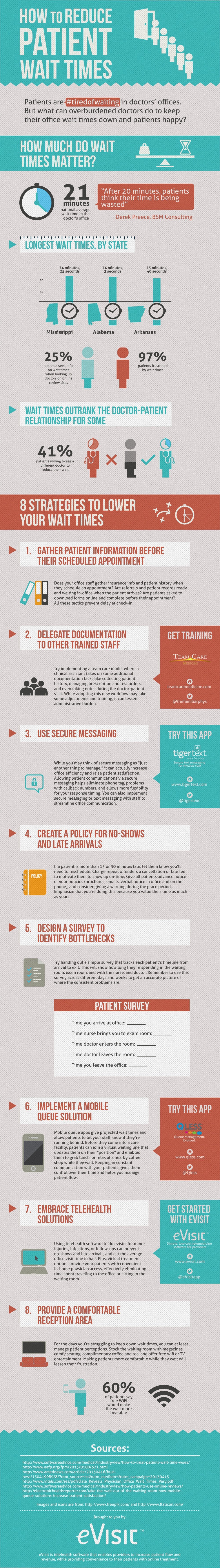
Your patients should be able to travel a clear path and really complete their visit, without needing to follow up outside the office. Try diagramming out the process so you can see any problems visually. If you’re having trouble tracking the flow for an average patient and pinpointing bottlenecks, try giving patients a simple survey to fill out as they cycle through the office.
Making patients' visits more efficient starts with your staff workflow. For example, do your front desk staff ask the same questions of every patient? If so, they could be gleaning unnecessary information for some patients, and not enough for others. After all, a patient coming in for follow-up has different needs than someone considering extensive procedures. Your office staff and practitioners can avoid unnecessary double-questionings by developing different intake paperwork for different types of visitors.
-
Does everyone in your office know their duties?
This is the opposite of in-office redundancy: the classic "I thought Jim did that" situation. It slows the whole office down when a staff member has to track down a doctor who didn't provide information necessary for billing, or when an EMR entry looks spotty because chunks of data are absent. When your staff has specific duties, it's much easier to distribute resources and estimate time commitments, and it doesn't leave any last-minute scrambling at the end of the day.
At Medical Economics, Brandon Glenn advocates for departmental checklists, which can be especially helpful during transitional times, such as when you're adjusting to a new EMR. Glenn's suggestions are based on a BMJ Quality & Safety article that found task lists effective in practices big and small. To improve primary care office workflow in your practice, assign generic tasks like "gather information" to different staff departments, and help develop specific subtasks that can be assigned to individuals.
[thrive_leads id='6994']
-
Can you draw a timeline of a day in your office?
In your practice, are tasks completed when people cross paths, or at a regular time every day? In medicine, it can be difficult to follow a rigid schedule, but there's still a limit to what can be done in a day—and it all needs to get done. It may be time to assess your practice's time management. A great example of this is phone messages. Jill Young at the American Academy of Family Physicians describes two common scenarios:
"Examine how often [phone] messages are delivered to staff. Do you have a Janie Jump Up? This would be the staff member who leaves her desk every time she has a message of any kind to deliver, leaving the phones short-staffed or unattended. Or do you have a Let It Wait Linda? She delivers messages at the end of the day – all of them, all at once. Staff who thought they were done suddenly are staring at work they had not budgeted for, possibly resulting in overtime expenses for the office."
Try to set timeframes in your practice that maximize total efficiency. If office staff can take turns delivering messages in morning, afternoon and evening phases, for example, you can make sure the phones never go unstaffed. You can use the same strategy for ordering tests, completing referrals, and other paperwork that often costs valuable time. Setting these deadlines enforces good habits and prevents in-office traffic jams.
-
Are communication lines clear, open and accessible to everyone?
The cornerstone of all these steps is communication. You don't just need specific duties; you need staff to know who does what. Patients can't be expected to know their visit timeline; they need guidance from staff along the way to make the most of their time in-office. No one can dictate what your office culture is like, but do make sure open communication is a major tenet. In the age of EMR integration, this is an especially important idea, since many doctors feel EMR technology detracts from face-to-face communication.
Even if members of your team don't work together directly, they should still feel comfortable communicating with one another, and be willing to critique and praise each other as well. One of the best ways to optimize health technology is to constantly reassess your processes, so encourage staff to make recommendations, and praise innovative solutions that streamline your office workflow.
[thrive_leads id='6445']
-
Can you clearly explain your billing process ?
No matter how many patients you have, or how many insurance providers you work with, there are a lot of places your billing can go wrong--and chances are, it will. The best way to avoid workflow-jamming billing problems is to understand your billing process inside and out. If your billing is done in-house, make billing a specific job, not an added responsibility for another staff member, says Michelle Rimmer on Kareo's Getting Paid blog.
Rimmer advises that the billing process should start at the front line--your desk staff--because patients start thinking about their bill even before they walk into your office. "It is imperative that staff at the front desk has some type of introductory insurance and/or billing training," Rimmer says. Make sure your desk staff can answer common questions about copays and payment processes. This is also where those open communication lines come in handy—your desk staff should be able to ask in-house or outsourced billing experts for help in talking to patients. Make sure your patients receive updates on any process or policy changes, too, to make transitional phases easier all around.
Like all parts of practice management, adjusting your workflow is a constant process. As your practice grows, technology updates and policies change, you'll need to tweak your systems to maximize treatment efficiency. Don't be afraid to make some major shifts, but do remember to change one thing at a time, so you can tell if new tactics are working. An efficient office means less stress for staff, which is good for patients, too.
When did you realize your workflow needed an overhaul? How did you fix it? Share your story with us!
[thrive_leads id='7258']